Williams syndrome can be associated with various issues related to the spine- lordosis and kyphosis being the most common; scoliosis being the least. Lordosis and kyphosis typically develop during adolescence and/or adulthood and are preventable. Scoliosis may develop late in childhood. Research on WS individuals with scoliosis indicates that it may be coupled with other inheritable mutations outside the WS area and are linked to familial inheritance.
Bends in the spine due to muscle tone
Lordosis is commonly called swayback. It is when the spine has a pronounced curve in the lower back, called the lumbar region which can cause a belly that sticks out further than normal. It is the most common postural issue in WS, found in 38% of individuals.
Kyphosis is also known as humpback. This is when the spine typically curves outwards towards the back of a person. This condition is most common in the upper back just below the shoulder blades and behind the chest. It is found in 20% of individuals with WS.

The causes of kyphosis and lordosis in WS are rooted in two issues- the missing elastin (ELN) gene and the muscle tone of the lower extremities. Elastin deletion is the underlying genetic mutation used to diagnose WS. Elastin is a protein found in many connective tissues of the body that give the tissue both strength and flexibility. It can work much like a spring, allowing the tissue to lengthen but bounce back and retain its original structure. It is found in virtually every organ in the body and arranged in a way to improve the function of the structure. For example, it is found in rings around the arteries, in strips down a ligament or in net like sheets within the skin.

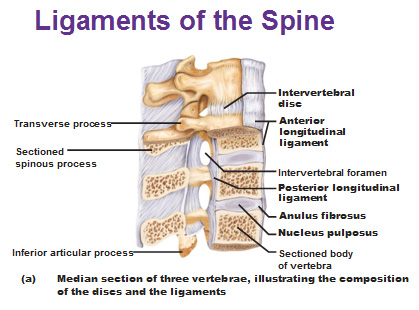
Most notably in kyphosis and lordosis, the lack of elastin can cause ligaments that support the vertebrae to loose their strength. There are several sets of ligaments that cradle the vertebrae. The anterior longitudinal ligaments run long ways down the body of the vertebrae. This is the section of the vertebrae most central to the body, or towards the front. The posterior longitudinal ligaments run beneath the spinal process or points of the spine on the back side of the vertebrae. This is the area that you would touch if you ran your hand down your back. Both of these sets of ligaments are arranged with a connective tissue called dense regular tissue. This tissue has long sections of collagen and elastin that are packed tightly together and all run in the same direction. This allows some give to the ligament but due to the direction of the fibers, gives strength in the direction of the primary force (supporting the weight of the body on the pelvis). When there is less elastin, the ligaments become looser and strength is reduced. This can cause the vertebrae to slip out of alignment and compress the intervertebral discs in an abnormal fashion.
The second issue with kyphosis and lordosis is muscle contractures or high tone in the lower extremities. Contractures are tightening of muscles due to increased tone. The contraction of the muscle pulls with extra force on tendons. This in turn can pull on bones and create an uneven posture, affecting bone alignment and the development of kyphosis or lordosis. It is important for individuals with WS to monitor their muscle tightness, especially in the legs and hips and to stretch them so that contractures do not get severe and cause further debilitating symptoms. (See my blog post on muscles for more information on this.) The prevalence of lordosis and kyphosis in WS is attributed to the muscle contractures that often occur in the lower body, particularly the hips, and lax joints due to the missing elastin in the ligaments of the spine.
The tightening of the muscles are much more common in adults with WS than in children and postural issues tend to be very mild. These conditions are preventable through physical therapy. Typically children with williams syndrome receive physical therapy at an early age but as they reach adolescence that service often ceases. It is suggested that adults with WS get physical therapy evaluations occasionally to determine if kyphosis or lordosis is occurring due to tight muscles in the lower body. Stretching the tight muscles is the easiest and best preventive treatment you can take to avoid these issues. If muscles become very tight, it is important to get further treatment from a physical therapist and to see orthopedics. Some individuals will be fitted with orthodics that are designed to sustain a long stretch, sometimes overnight to treat the muscle. Nurturing muscle health is the primary way to treat kyphosis and lordosis related to WS.
Scoliosis
Unlike kyphosis and lordosis being the prevalent postural issues in WS adults, some individuals are born with or develop scolisis at a young age. Scoliosis is a curvature to the side. These can often be in a C shape or S shape. It is found in 12% of individuals with WS, which is considered a low incidence and typically presents itself by the 8th birthday.
Scoliosis is known in the general population to be caused by a mutation on the fibrillin 1 (FBN1) gene, which is NOT in the WS region. It is found on chromosome 15. In all individuals with scoliosis in the general population, research indicates that this mutation accounts for 60% of cases. FBN1 is known to affect the ability for the body to properly create strong elastin. This is similar to the WS deletion which affects elastin's ability to bounce back under stress. The difference between the two causes of scoliosis is that those with the FBN1 mutation are more likely to develop scoliosis than those with WS, showing that the FBN1 gene more negatively affects elastin's strength in terms of spinal development. .
In Williams syndrome, scoliosis can be linked to a specific gene mutation in conjuction with the classic deletion in the WS region. The mutation is on a gene called SERPINA1. SERPINA1 is a gene that is responsible for creating a protein called α-1-antitrypsin (AAT for short). An AAT mutation is relatively common in the general population. If a person inherits the mutation on both of their genes it can cause serious health issues such as emphysema and liver disorder, although, a double mutation is rare. Carriers of one mutated gene can also have adverse health issues, such as scoliosis. Since many people carry this mutation on the SERPINA1 gene, it is possible that some individuals with WS would also be carriers. Researchers believe that this is the connection between a low incidence of scoliosis with WS.
AAT is a protein that is an inhibitor of an enzyme. Enzymes are proteins that help speed up reactions within the body. Without them our body would not be able to survive. The functioning of the body is basically a collection of complicated chemical reactions. Most of these chemical reactions wouldn't take place fast enough for us to survive so we have proteins called enzymes that reduce the amount of energy needed for those reactions to take place. We have thousands of enzymes in the body, each made to help speed up one particular reaction that we rely on for survival.

The AAT protein affects an enyme called elastase. Elastase is used by the body to reorganize elastin in the connective tissues. When the body is laying down elastin in large amounts, usually during rapid growth at the end of pregnancy and throughout the first year of life, the body undergoes large amounts of physical stress. This stress can create some inflammation within tissues, such as connective tissue. The body's response to this is to repair the tissue by breaking down the damaged elastin fibers and replacing them with new. The enzyme used to break down the elastin is elastase.
With every enzyme it is important for the body to have a counteractive protein to control its reactions. Enzymes are renewable meaning after they perform their desired reaction, they can disconnect from the substrate (or molecule they are breaking) and work on another. In the case with elastase, it would break down a portion of elastin and then disconnect and work on another. Therefore, the body makes a second protein, called an inhibitor, that slows down or stops the action of an enzyme within the body. This is the body's way of preventing too much degradation of the elastin proteins. When an individual has a mutation on the SERPINA1 gene, they fail to make enough of the AAT protein which is elastase's inhibitor. This means that their body can not slow down elastase from destroying elastin, causing an absence of elastin in areas of the body such as the joints.

The destruction of elastin by AAT coupled with the inability to make elastin by the WS deletion is thought to be the main reason why some individuals (about 12%) with WS have scoliosis. The lack of the elastin compromises the structure of the discs that are in between the vertebral bones that function to cushion the vertebrae. An intervetebral disc is structured with a ball-shaped section of cartilage that is in the center, called the nucleus pulposis. This area of the intervertebral disc is very dense with elastic fibers that are designed to compress and absorb stress from the weight of your body on the vertebrae. In fact, over the course of a day the discs are said to actually be thinner than when you first wake up. This is the nature of the elastin, absorbing the force and then springing back to it's original shape. Circling around the nucleus pulposis are rings of connective tissue called the anulus. The anulus has connective tissues thick with collagen (fibers designed for strength) that alternate with rings of elastic fibers for flexibility. As you get closer to the center of the rings, the elastic fibers increase in number and are organized in a way where they sit against each other in different angles than its neighboring rings. The structure of these layers reflect the function of the disc (giving it strength from pressure in various directions).

Knowing the structure of intervertebral discs, it's not surprising to find that the lack of elastin can devastate the integrity of the structure. When a child goes through stages of rapid growth, the intervertebral disc, the bone in the spine and the ligaments that support those structures undergo a drastic change in force placed on them by the body. This can cause stress on the tissues and minor injuries. The distressed tissue will release chemicals indicating that it is injured, activating elastase, the enzyme designed to destroy elastin. If a individual has the AAT mutation, it is difficult for their body to reduce or stop this enzyme action resulting in lower levels of elastin in the body. Coupled with the inability for the body to make adequate amounts of elastin (due to the WS ELN deletion), the intervetebral discs and ligaments can lose their strength and fall out of alignment, resulting in curvature of the spine- scoliosis.
The spine or vertebrae are normally positioned in a way that they sit directly over the pelvis. Their primary function is to protect the spinal cord but they also contain a large base that absorbs much of the body's weight and allows us to stand erect and walk on two legs. When the spine is displaced such as in these issues, it can cause back pain, putting additional stress on the muscles of the back, and awkward gait when walking since the body is not positioned properly in line with the pelvis.
Other rarer conditions related to the spine
Some WS individuals may develop kyphoscoliosis which is a combination of kyphosis in the upper back and scoliosis. This condition is often due to having hypertonic (high tone in the legs and hips) coupled with hypotonia in the core of the body (low tone of the muscles). In addition to the unbalanced tone in the muscles, the muscles have a lax nature due to elastin deficiencey in the tendons that attach them to the spine and in the ligaments that connect each vertebrae to one another. Rarely if this occurs there can be a large curvature inwards that puts pressure on the heart and lungs and could create a need for surgery. Incidences of this occurring are all recorded in children.Treatments of scoliosis
Doctors and schools typically check for scoliosis between the ages of 8 to 10. They will often look at the curvature of the spine by having the child bend and touch their toes. If scoliosis is suspected, x rays will follow to determine if there is a degree of curvature. Anything less than 25 degrees is typically not treated, just followed to be sure it doesn't progress. If the curvature is 25-30 degrees, a back brace may be fitted. Curves greater than 30 degrees will often lead to surgical repair where they fuse the vertebrae or insert metal rods to support it. Surgery and treatment is always determined based on the patient, their needs and how much growth they still have in their future.
Sources used:













