The lacey pattern can be found in the general population (about 10%) so it is not considered an abnormality, rather its a unique version or phenotype of the iris. The iris is the colored portion of the eye. It is an extension of the white of the eye, called the sclera, and is completely surrounded by a liquid called humorous. Just under the iris sits muscle, or ciliary bodies, that control how light is focused toward the back of the eye. Muscles in the iris control how much light enters the inside of the eye by changing the size of the pupil or opening (the black of the eye).
Although it is somewhat of a mystery as to why the lacey or star burst pattern is found so frequently in WS, studies have linked the pattern to some structural traits of the iris tissue. The iris of the eye is made up of 4 layers or tissues. Slight changes to the second layer seem to contribute to the lacey pattern. The second layer of tissue is called the stroma. The stroma is a mesh of fibrous tissue that is filled with blood vessels, nerves, and immune cells called macrophages. The top of this thick layer in the iris contains trabeculae. Trabeculae are tiny channels that drain fluid in the eye and maintains its pressure. Often, in WS, these channels are raised up higher and sit more prominantly than in a typical eye. Also, scientists have found that this section of the eye has a decreased growth of cells, called hypoplasia, during growth as an embryo. This contributes to the starburst pattern as well.
The base of the stroma is made up of two muscles that control the shape of the iris. If the lighting in the environment is dark, the muscles relax and open the pupil (hole) wider to let in more light. If the lighting is bright, the muscles contract to close the pupil and restrict the amount of light entering the eye. There is an area in the iris where the two muscles overlap, called the collarette. This is the thickest part of the iris. Studies have shown that WS causes this collarette to sit in a displaced location or become absent entirely, creating a sinus or dip in the tissue. This contributes to the starry pattern in the iris.
To prevent light from traveling through the tissue of the iris, pigment sits in the 4th layer. The pigment is determined by the amount of melanin in this layer. People with blue eyes have the least melanin and people with brown eyes have the most. You can think of melanin like an umbrella that sits over the outer surface of the cell. It shades the cell and absorbs the light so it cannot pass through. Interestingly enough, individuals with WS are about 70% likely to have blue eyes. The star burst pattern is best seen in blue eyed individuals although it does exist in green eyes and most likely covered up by pigment in brown eyed people. Studies have linked the starry pattern to 50-70% of individuals with WS, so it is used as a diagnostic clue or evidence of the syndrome.
Maintaining a clear picture
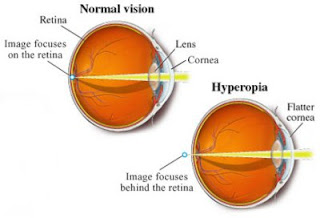
Many children (50%) with Williams syndrome tend to become far-sighted in early childhood. Far-sightedness is called hyperopia in the medical world. When a person is far-sighted, they tend to see objects well from a distance but have trouble focusing on something near.
An example of what a close object might look like to someone with hyperopia.
It is easy to understand what happens in hyperopia when you understand how the eye works. When light bounces off of an object in the environment, it passes through the clear window on the front of your eye called the cornea. The cornea is the first structure designed to focus the light and direct it into the pupil, or hole, which leads light to the interior of the eye. Just behind your pupil sits a round, clear ball of fibers called the lens. The lens is flexible. It is attached to muscles that pull and change the its shape to focus the light onto the back of the eye. On the back of the eye sits a thin membrane called the retina. The retina has 7 million tiny light receptors called rods and cones that pick up the light signal and talk to the optic nerve. The nerve then sends the information to the brain for interpretation. It is important for the light to focus properly onto a small area of the retina called the fovea centralis. This is the part of the retina that contains the majority of the cones.
Hyperopia can be caused by one of two things. First, the cornea of the eye, or the clear outer portion where you would put a contact lens, has a slight curvature. In other words, it's flatter than normal. It can also be caused by people who have a short eyeball. Both of these abnormalities cause the light to focus at a point behind the retina. This causes the light to scatter over a larger area of the retina instead of at the fovea centralis. The scattered light does not provide a clear picture for your brain to interpret and you end up with blurry vision.
Hyperopia is simple to treat. You would be prescribed glasses. Glasses are basically a lens that bends the light before it enters your eye. So they aid the structures in your eye that are designed to focus the light, such as the cornea.
Seeing Straight
50% of children with Williams syndrome encounter an issue called esotropia. Esotropia is due to one or more eyes being misaligned or crossing inwards towards the nose bridge. When the eye is misaligned, the child will end up seeing double. If you've ever played around and crossed your eyes for fun, you'd understand what that would be like. This is essentially what your child would be seeing. When the brain receives this visual input, it has to accommodate in order to navigate its surroundings.
There is a difference between crossed eyes and lazy eyes...
As esotropia progresses, the brain can become confused by the images that it receives. In order to restore proper vision, it will often choose one eye's image and "turn off" or ignore the other. This would be like you closing one eye and just functioning with partial vision. This is called amblyopia or lazy eye. When this occurs, the person loses their depth perception and the condition can cause spatial issues. If the vision is not corrected right away, this will become permanent and their vision will not be regained. Therefore, as soon as you notice a child's eyes are misaligned, it is important to see a pediatric opthamologist. Just the slightest misalignment can cause major problems down the road. The sooner the condition is treated, the better the outlook of maintaining good vision for your child.
When a child's eyes are misaligned it is important to treat them for amblyopia. This is a preventive measure to encourage the body not to turn off the images from the weaker eye. This is accomplished by patching. A patch, that looks similar to a band-aid, is placed over the stronger eye (the one that stays properly aligned) for a prescribed length of time during the day. The purpose of this is to force the brain to use the weaker eye for visual input and to train the brain not to turn off that vision. Some opthamologists will prescribe an eye drop that muddles the vision of the strong eye if patching is unsuccessful. There is a lot of information on the internet about a practice called vision therapy. Vision therapy is rarely prescribed by an opthalmologist and rarely, if ever, covered by insurance because there is no scientific evidence that it actually works.
It is important to understand that amblyopia or lazy eye is NOT the same as esotropia. Lazy eye is caused by estropia, therefore they have to be treated separately and treated as two different conditions. There are two types of esotropia, both with different causes.
Infants with esotropia
If the esotropia presents itself when the child is very young (typically before their 6 month birthday) it is caused by muscle weakness of the eye. The eye is surrounded with several sets of muscles that control the direction that the eye moves. The muscle that is found on the inside of the eye is called the medial rectus muscle. In many infants with WS this muscle can be weak or hypotonic. Hypotonia is not necessarily due to how physically strong the muscle is, but due to the brain's ability to control the muscle. Therefore, infantile estropia is often found in children with mental delays, as in WS.
Eye muscle surgery is a simple outpatient procedure. The patient is sedated (see the WSA website for anaesthesia issues) and the doctor manipulates the eye to turn it outward, exposing the medial rectus muscle. The outer layer of the eye where the muscle attaches is cut and the muscle is sewn back onto the eye in the proper place, realigning the eye. The difficulty with the surgery is that the surgeon literally "eye balls" where to sew on the muscle. All individuals have their own eye shape and muscle length so there really isn't a measurable distance to sew the muscle on. This makes the success rate 80%.
Many patients have to have the surgery multiple times in order to maintain the proper alignment. There are also some surgeons that use adjustable sutures but these are most common in surgeries for adults. The sutures can be adjusted in the office post surgery if the eye is still misaligned. Typically, if the eye is still misaligned another surgery will be scheduled for 3-4 months later and patching is prescribed in between to maintain the vision in the weak eye. Subsequent surgeries have the same success rate so some children will need it a 3rd time. (My daughter had this surgery and it was successful after the third operation).
Just a note about the surgery recovery. It doesn't cause any pain. It is said that it feels like dust is in your eye. The eye is very red for a week or two until the tissue cleanses it but our daughter played when she returned from the hospital and went trick or treating the following day which was Halloween.
Esotropia in older children
If a child is far sighted, they can actually develop esotropia over time. If hyperopia or far-sightedness is not corrected in children, or their prescription needs updating, their eyes will tire from squinting and trying to see clearly. The fatigue can cause one eye to fall or cross inward. This is called accommodative esotropia.
When you see an opthamologist for this condition, they will test the child for hyperopia and fit them with glasses. The glasses should fix the issue because the brain no longer has to accommodate for the failed vision. If the child takes off their glasses, the eye may fall back in misalignment again because the brain has to accommodate once more. Patching may also be prescribed in order to prevent amblyopia from developing.
Overtime, the condition should correct itself. As people age, far-sightedness decreases and the accommodation of the esotropia would disappear.
What to do if you notice issues with your child's vision?
As far as vision goes, the earlier that the condition is identified and seen by a pediatric opthamologist, the better. Poor vision can affect their ability to develop and learn, even from a very young age. By providing them with good vision care, you are optimizing their potential.
Sources:
Stabismus in Williams Syndrome
Ocular features of Williams Syndrome
The iris in Williams Syndrome
Sources:
Stabismus in Williams Syndrome
Ocular features of Williams Syndrome
The iris in Williams Syndrome